The following article does not reflect changes in protocol in light of COVID-19. For more detailed information as to how our office has gone Sterilization & Disinfection above and beyond basic recommendations as a result of the pandemic, please visit our article/blog using the following link.
At Dental Lavelle, we strive to deliver high-quality care. Our protocol for infection control, Sterilization & Disinfection, and prevention is of the highest importance for the safety of our patients, our team, and the community.
Transmission of infectious agents among patients and dental health care personnel (DHCP) in dental settings is rare, however, there have been a few reported cases in the United States. In most cases, investigators failed to link a specific lapse of infection prevention and control with a particular transmission. A comprehensive protocol with a number of different systems integrated together would offer the best protection.
At Dental Lavelle, we follow “Guidelines for Infection Control in Dental Health Care Settings” recommended by the Center for Disease Control and Prevention (CDC), USA.
Standard Precautions
Standard Precautions are the minimum infection prevention practices that apply to all patient care, regardless of suspected or confirmed infection status of the patient, in any setting where health care is delivered. These practices are designed to both protect DHCP and prevent DHCP from spreading infections among patients. Standard Precautions at Dental Lavelle include:
- Hand hygiene.
- Use of personal protective equipment (PPE)(e.g., gloves, masks, eyewear).
- Cough etiquette.
- Sharps safety
- Safe injection practices (i.e., aseptic technique for parenteral medications).
- Sterile instruments and devices.
- Clean and disinfected environmental surfaces.
Each element of Standard Precautions are described in the following sections.
1. Hand Hygiene
For routine dental examinations and nonsurgical procedures, we use water and an antimicrobial soap (hand antisepsis) specific for health care settings. For surgical procedures, we perform a surgical hand scrub with an iodine based surgical antiseptic soap after which we put on sterile surgeon’s gloves.
2. Personal Protective Equipment

3. Cough Etiquette

4. Sharps Safety

Most percutaneous injuries (e.g., needlestick, cut with a sharp object) among DHCP involve dental burs, needles, and other sharp instruments. Implementation of standards has helped to protect DHCP from blood exposure and sharps injuries. However, sharps injuries continue to occur and pose the risk of bloodborne pathogen transmission to DHCP and patients. Most exposures in dentistry are preventable Sterilization & Disinfection. We take precautions while using sharps, during preparation, during use, during cleanup, and during disposal.
Some practice controls include not bending or breaking needles before disposal, not passing a syringe with an unsheathed needle by hand, removing burs before disassembling the handpiece from the dental unit, and using instruments in place of fingers for tissue retraction or palpation during suturing and administration of anesthesia.
All used disposable syringes and needles, scalpel blades, and other sharp items are placed in appropriate puncture-resistant containers located in each operatory. Dental Lavelle has partnered with a certified vendor for safe disposal from the dental practice on a frequent basis.
5. Safe Injection Practices
Safe injection practices are intended to prevent transmission of infectious diseases between one patient and another, or between a patient and DHCP during preparation and administration of medications. Safe injection practices are a set of measures we follow to perform injections in the safest possible manner for the protection of patients. When administering local anesthesia, during which needles and cartridges containing local anesthetics are used for one patient only. All needle’s we use are disposed after every single patient and not re-used. The delivery system we use is either a single use disposable one, or a metallic dental cartridge system that is heat treated (autoclaved per the manufacturer’s instructions) after every patient.
6. Sterilization and Disinfection of Patient Care Items and Devices
Instrument processing requires multiple steps using specialized equipment. We have policies and procedures in place for containing, transporting, and handling instruments and equipment. Most single-use devices are labeled by the manufacturer for only a single use and do not have reprocessing instructions.
Patient-care items (e.g., dental instruments, devices, and equipment) are categorized as critical, semicritical, or noncritical, depending on the potential risk for infection associated with their intended use. Critical items are sterilized using heat treatment, while semi-critical items are sterilized using heat treatment or a high level of chemical disinfection. Noncritical patient-care items (e.g., x-ray head / cone, blood pressure cuff, etc) are those that only contact intact skin. These items pose the least risk of transmission of infection. In the majority of cases, cleaning followed by disinfection with a hospital disinfectant is adequate.
For the above items, the first step is rinsing and scrubbing to remove debris. Subsequently, the items are placed in an automated system called an ultrasonic cleaner. During this timed ultrasonic cleaning, the items are soaked in a multi-enzyme cleaning solution to digest organic biological residue.
After cleaning, the instruments are dried, inspected, wrapped, and packaged (or placed into container systems) before heat sterilization. The instruments are then placed in a Class B autoclave and steam heated per industry standards for sterilization (triple vacuum cycle at 121C with 15 psi pressure with a minimum cycle time of 15 minutes) using distilled water manufactured with an on-site distillation plant. The ability of a sterilizer to reach conditions necessary to achieve sterilization should be monitored using a combination of biological, mechanical, and chemical indicators.
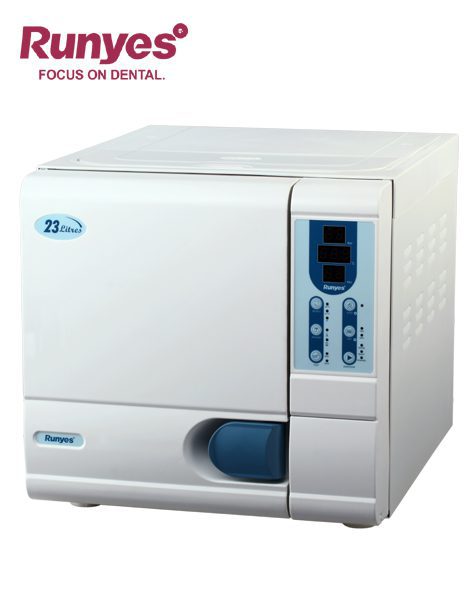
Mechanical monitoring involves checking the sterilizer gauges, computer displays, or printouts; and documenting the sterilization pressure, temperature, and exposure time in sterilization records. Chemical monitoring uses sensitive chemicals that change color when exposed to high temperatures or combinations of time and temperature. Chemical indicators also help to differentiate between processed and unprocessed items, eliminating the possibility of using instruments that have not been sterilized.
Wrapped packages of sterilized instruments are inspected before opening and use to ensure the packaging material has not been compromised (e.g., wet, torn, punctured) during storage. The contents of any compromised packs are reprocessed (i.e., cleaned, packaged, and heat-sterilized again) before use on our patients.
7. Environmental/Surface Infection Prevention and Control

Emphasis for cleaning and disinfection are placed on surfaces that are most likely to become contaminated with pathogens, including clinical contact surfaces in the patient-care area. Although hand hygiene is the key to minimizing the spread of microorganisms, clinical contact surfaces are barrier protected (disposable), cleaned and disinfected between patients. Hospital grade disinfectants are used for disinfection at Dental Lavelle. We partner with ‘Septodont’, a global leader with high quality products for the dental industry (Ex: Dermafilm, Dimenol, and Surfasept S.A.) with over 85 years of R&D and manufacturing.

Some surfaces within the operatory have undercuts and hidden areas that are easily contaminated and are difficult to clean (example: dental chair switches, overhead light handles, instrument tray handles, etc). We use disposable barrier tapes for every patient. At the end of a procedure, they are disposed of, area wiped down with a surface disinfectant, and a new set of barrier tapes are applied prior to seating the next patient.
8. Dental Unit Water Quality
Dental unit waterlines (i.e., plastic tubing that carries water to the high-speed handpiece, air/water syringe, and ultrasonic scaler) promote bacterial growth and development of biofilm due to the presence of long narrow-bore tubing, inconsistent flow rates, and the potential for retraction of oral fluids. Dental health care personnel and patients could be placed at risk of adverse health effects if water is not appropriately treated.

All dental units at Dental Lavelle use systems that treat water to meet drinking water standards. All independent reservoirs are filled with RO water.
During surgical procedures, we use only sterile solutions as a coolants/irrigant using an appropriate delivery device, such as sterile tubing that bypasses dental unit waterlines, or sterile single-use devices.
Maintaining correct practices of infection control and prevention are at the heart of Dental Lavelle’s operations. Our Doctors, specialists and staff are trained to do their best to provide dental care in a safe and pleasant environment. We dedicate time and resources to preparing the operatory for every patient, prior to and after every procedure done at Dental Lavelle. Safety is our priority!
If you have any questions or queries, please feel free to contact us.